Showing all 3 results
Introduction to Glaucoma
A medical condition where build-up pressure in the eye causes damage to the optic nerve is referred to as a patient suffering from Glaucoma eye illness. The optic nerve plays a very major role in transmitting visual information from the eye to the brain for further actions. The primary cause of Glaucoma is either an increase in intraocular pressure due to numerous reasons or trauma to an optic never.
Glaucoma is classified into two different types:
- Open-angle Glaucoma: This is one of the most common variants of Glaucoma. Such a medical condition occurs when the drainage tubes in the eye get clogged over time which results in causing damage to the optic nerve due to increased pressure in the eye.
- Angle-closure Glaucoma: It is a rare medical condition that occurs when the iris (the colored area of the eye) becomes too near to the drainage angle obstructing it and causing pressure to rise rapidly.
TRIVIA: Do you know?
Glaucoma is one of the leading causes of blindness among older adults. However, Glaucoma cannot be reversed but regular treatment can help maintain eye pressure to avoid future damage to the optic nerves causing permanent blindness.
Glaucoma can sometimes go unnoticed unless visibility becomes a major challenge. Family history with Glaucoma people should examine their eyes at least once a year. It is said that Open-angle Glaucoma patients most often have a family history of the same medical case. Periodic eye checkups will help early detection of any kind of eye illness and immediate treatment at a very early stage.
Most often Glaucoma treatment includes one or a combination of treatments. Eye drops or medications may be prescribed to maintain eye pressure while surgery may be carried out in order to prevent future damage to nerves.
Most often treatment like eye drops, oral medications, laser therapy, or surgery can help maintain eye pressure and prevent future damage to optic nerves.
Glaucoma in medical terms and its cause
The most common cause of a rise in intraocular pressure in the eyes is due to build-up of fluid in the eye that does not drain adequately.
The fluid, known as aqueous humour, is produced by the ciliary body and passes through the pupil to nourish the eye before draining out through the trabecular meshwork, a mesh-like network of tissues.
If the trabecular meshwork becomes obstructed or malfunctions, fluid cannot drain causing pressure to build up inside the eye.
Not all cases may be similar in some cases people with normal or low intraocular pressure can also suffer from Glaucoma. In these cases, the reason the optic is never may get damaged is due to various factors such as poor blood flow to the optic nerve or a weakness in the structure of the optic nerve, or Trauma.
There are higher chances of some with a family history, high intraocular pressure, near sightedness, African American or Hispanic ethnicity, medical illness such as Diabetes or high blood pressure or old age may suffer from Glaucoma.
Diagnosis and treatment
There are several tests that can be used to check for Glaucoma. These tests may include:
- Tonometry: This test helps to identify the pressure inside the eye. The process of Tonometry includes applying a small amount of pressure onto the surface of the eye and measuring the buildup pressure with the help of an instrument called a tonometer.
- Ophthalmoscopy: This test includes a close examination of the optic nerve with the help of an instrument called an ophthalmoscope to identify the signs of damage.
- Perimetry: This test helps identify the visible spot and blind spots in patients suffering from Glaucoma. In this test, a patient will be asked to look straight ahead while small lights or other stimuli are located at different positions or in a moving manner within the visibility of the eye.
- Gonioscopy: This test includes placing a special lens on the surface of the eyes allowing the doctor to examine the drainage angle in order to identify if it’s open or closed.
- Pachymetry: This test helps in measuring the thickness of the cornea. Corneal thickness can affect the accuracy of intraocular pressure measurements.
Apart from the test, your doctor may also evaluate your medical history, family history, and other risk factors that may contribute to glaucoma. In case Glaucoma is diagnosed, determining the severity of the condition treatment plan can be figured out in order to manage the disease and prevent further vision loss.
Treatment options for Glaucoma
The most common treatments for glaucoma include:
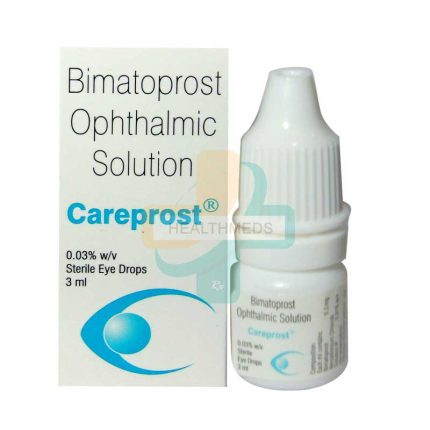
- Eye drops: The first line of treatment to manage the pressure inside the eyes is eye drops. They either work as reducing the amount of fluid produced in the eye or improve drainage.
- Oral medications: To reduce intraocular pressure oral medications may be prescribed along with eye drops.
- Laser therapy: If necessary, Laser therapy may carry out in order to improve drainage or reduce the amount of fluid produced in the eye.
- Surgery: If eye drops or laser therapy aren’t effective in controlling intraocular pressure, surgery may be recommended to create a new drainage channel for the fluid to leave the eye.
The most commonly used types of eye drops for glaucoma include:
- Prostaglandin analogs: Eye drops such as latanoprost, bimatoprost, and travoprost help increase the outflow of fluid from the eye. so that the eye pressure can be maintained.
- Beta-blockers: Timolol and betaxolol are very good examples of Beta-blocker drops that work by decreasing the production of fluid in the eye.
- Alpha agonists: Brimonidine and Apraclonidine some commonly prescribed eyedrops to patients suffering from Glaucoma that reduce the amount of fluid produced in the eye and increase the outflow of fluid.
- Carbonic anhydrase inhibitors: Carbonic anhydrase inhibitors used for glaucoma include a list of some good eye drops such as Dorzolamide and Brinzolamide that work by reducing the production of fluid in the eye.
- Rho kinase inhibitors: Eye drops such as Netarsudil and Ripasudil work by relaxing the muscles in the eye and increasing fluid outflow.